 Clinical Health Technologies has released a new mouthwash – Clinisept+. Dr Neil Millington discusses this new product, its history, chemistry and why his experience of using it over the last 15 months has convinced him it really is a game-changer for both dentists and patients.
Clinical Health Technologies has released a new mouthwash – Clinisept+. Dr Neil Millington discusses this new product, its history, chemistry and why his experience of using it over the last 15 months has convinced him it really is a game-changer for both dentists and patients.
Do we need a new mouthwash in dentistry?
Dentists prescribe mouthwashes to patients in order to provide fluoride or to act as an antimicrobial agent. Mouthwashes come in all shapes and colours. But the vast majority of them contain chlorhexidine. This has been the staple chemistry of mouthwash formulations for around 50 years.
Dentists continue prescribing these mouthwashes in large quantities. That’s despite wide acknowledgement that they have several drawbacks. Patients report a harsh taste and lingering and long-term use can cause changes in taste sensations. Plus there is the problem of it causing teeth staining. In some patients this can be severe enough to require remedial action in itself. Indeed, it is sometimes said that the only benefit of chlorhexidine is that the level of staining is a good indicator of patient compliance! Chlorhexidine is certainly not an ideal mouthwash for anything other than short-term use.
In terms of its effectiveness, at 0.2%, chlorhexidine is antibacterial but delivers modest levels of disinfection against fungi and viruses and is ineffective against bacterial spores. But like so many of the ‘traditional’ skin disinfection technologies, it isn’t especially skin compatible. Any Google search will detail the dangers of the chemistry. These include health hazard, irritant and environmental hazard symbols. The BNF lists common or very common side effects of intraoral use of chlorhexidine as dry mouth, hypersensitivity and taste alteration. Sensitivity to chlorhexadine varies. In 2012, the Medicines and Healthcare products Regulatory Agency (MHRA) issued a warning about the risk of chlorhexidine causing anaphylactic reaction and in 2017 the US FDA reiterated a similar concern. The British Dental Journal (Pemberton and Gibson, 2012) reported two cases of death following type one anaphylactic reactions to chlorhexidine.
But is there any viable alternative to chlorhexidine?
Actually, yes! It now appears there is.
Clinisept+ Mouthwash is a new ultrapure hypochlorous solution. A chlorine-based solution, it has a whole raft of highly desirable characteristics. It is an incredibly effective disinfecting agent (being bactericidal, fungicidal, virucidal and sporicidal in seconds – and many times more effective than hypochlorite), yet, uniquely, it also has a skin neutral pH (making it harmless to enamel), is non-toxic, non-irritant to the oral mucosa, and, is also non-cytotoxic.
Hypochlorous therefore offers an ideal combination of very rapid (within seconds) destruction of bacteria (and therefore protection against infection) via its strong oxidising action, whilst being completely skin safe. A key reason for this compatibility with human tissue is that hypochlorous is actually produced by our own immune system during the phagocytosis of pathogens by neutrophils. Importantly, this oxidation process is not subject to antimicrobial resistance.
A brief history
A chlorine-based chemistry, the first proven effective antiseptics were hypochlorus solutions. Dakin’s solution (0.5% sodium hypochlorite) offered spectacular results to irrigate and dress traumatic wounds during the First World War. EUSOL (Edinburgh University Solution of Lime) followed this. This was used for the management of open wounds left to heal by secondary intention.
Although first reviewed in the BMJ in 1915 (Smith et al) hypochlorous solutions have not, until now, seen widespread use within medicine and dentistry. This is due to it being very difficult to produce a hypochlorous solution of sufficient purity. A purity that truly delivers the desired characteristics of ‘super effective disinfection’ (bactericidal, fungicidal, virucidal and sporicidal) and extreme skin compatibility (skin neutral pH, non-irritant and non-cytotoxic). When high purity of hypochlorous (HOCL) is not achieved (as has been the case to date), high proportions of hypochlorite (OCL) are present. This makes it neither nearly as efficacious in disinfecting and nor is it safe for contact with the skin. Bleach for example is nearly all sodium hypochlorite and highly alkaline with a pH as high as 13. This enables its ‘germ’ killing properties. However, this makes it completely unsuitable for use on skin and mucosa.
Limitations
Purity is not the only challenge in the manufacture of hypochlorous. In its natural state, hypochlorous has a half life of only 48 hours, rendering it very difficult to commercialise.
Until now, the quality of hypochlorous available for general use has been highly variable. As a result, it has seen limited use in human healthcare applications. That’s despite extensive documents showing its potential benefits. One of the few areas where it has seen good use is for the process of sterilising delicate medical instruments such as endoscopes. But, due to the challenges above, these solutions required daily replacement and only contained a maximum of 50% hypochlorous content.
Changing the hypochlorous landscape!
Now however, the advent of Clinisept+ technology, has completely changed the hypochlorous landscape. Clinisept+ contains over 90% pure hypochlorous, yet has a shelf life of more than two years. A proprietary manufacturing process achieves this. It uses hypochlorite as an active ingredient, but then converts the hypochlorite into a solution of almost 100% hypochlorous.
This means that Clinisept+ Mouthwash is probably the most potent antibacterial, antifungal and antiviral solution available that is also non cytotoxic and non-irritant to the skin and oral mucosa. It has a long shelf life for use as both a short and a long-term mouthwash. All without any of the drawbacks associated with the use of chlorhexidine.
The author’s experience of using Clinisept+ Mouthwash over the last 15 months has been extremely positive. There has not been any unfavourable outcomes seen. Instead, results have exceeded expectations. Patient responses have only been positive, with nearly all patients much preferring to use Clinisept+ over chlorhexidine mouthwash. Results have been particularly impressive with treatment of ‘sore mouth conditions’ such as erosive lichen planus, aphthous ulcers and denture stomatitis. It is also effective in relieving pain and inflammation associated with pericoronitis when the solution is syringed beneath the operculum using a plastic cannula and syringe. Treating acute and chronic periodontal conditions effectively is possible using a combination of pocket irrigation with Clinisept+ after RSD (route surface debridement) and followed up by patients brushing with their toothbrush dipped in Clinispet+ and then daily Clinisept+ mouthwashes.
Comparing mouthwashes
The extent to which Clinisept+ appears to calm and stabilise the skin is in stark contrast to the author’s experience of a number of patients who have become sensitised to chlorhexidine. One such patient was prescribed chlorhexidine mouthwash over a prolonged period following upper and lower clearance, a lower same-day teeth procedure, plus the fitting of a full upper immediate denture in January 2016. Within a few weeks she had developed severe oral ulceration with spontaneous bleeding and severe pain (Figure 1).

The author suspected chlorhexidine as a cause and its use was halted. However, we treated the patient over the next two ½ years with both oral and systemic steroids and she continued to suffer. We recommended the use of Clinisept+ Mouthwash in October 2018. Within two weeks the patient reported her ‘mouth felt more comfortable than at any time during the previous two ½ years’. Figure 2 shows the patient four weeks after starting use of Clinisept+ Mouthwash. The patient has since continued to be comfortable and continues to use Clinisept+ on a soft toothbrush to clean her implants. She remains hypersensitive to general toothpaste and mouthwashes other than Clinisept+.

Using Clinisept+ mouthwash
In the surgical situation, we use Clinisept+ to ‘soak’ infected extraction sockets following removal of the tooth and curettage of the socket. We irrigate extraction sockets with Clinisept+ prior to placement of an immediate implant.
Post-surgical protocol includes twice daily 30-second mouthwash with Clinisept+ for two weeks. Prescribing antibiotics either pre or post-surgery is now routine. Intraoral healing is normally rapid in any case. So quantifying any reduced healing time due to Clinisept+ is difficult. However, I believe patients report less pain than experienced when chlorhexidine was previously used as part of post-surgical regimen. There is no doubt that patients previously using chlorhexidine post-surgery, much prefer Clinisept+.
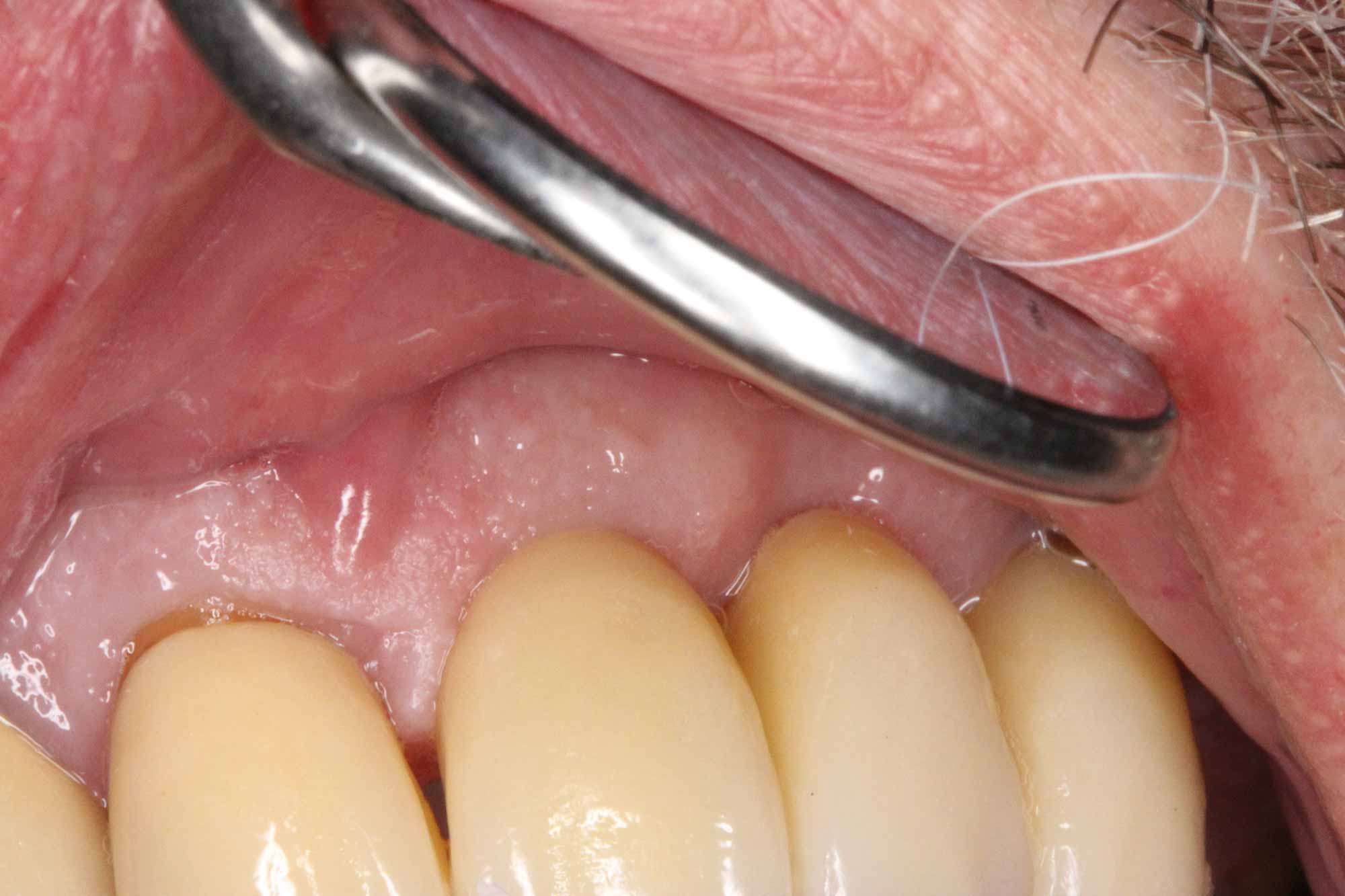
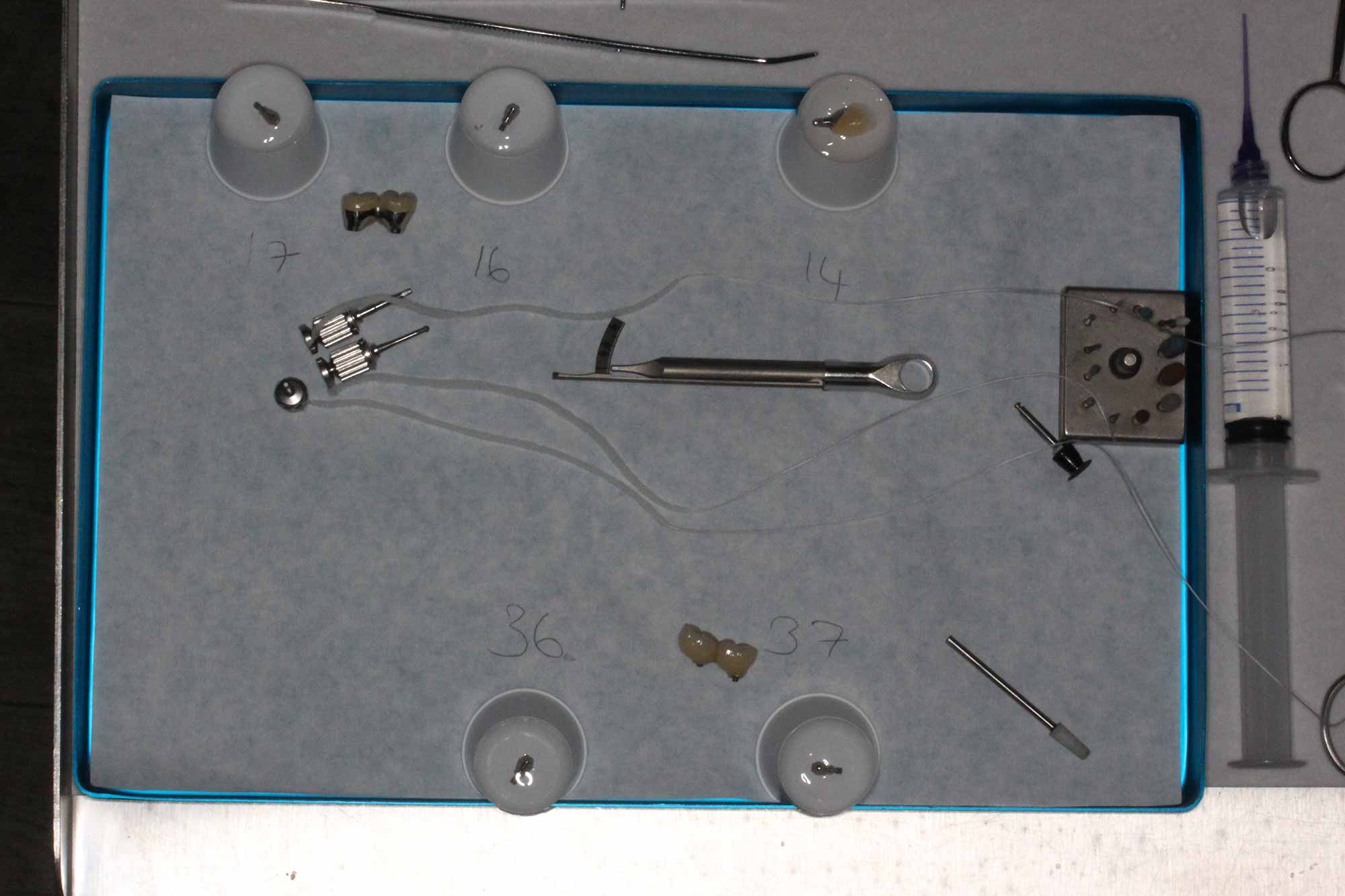
During the restorative stage of implant treatment, each time we remove a healing abutment, the internal access to the fixture is irrigated with Clinisept+ (Figure 3).

When provisionally filling screw access holes of implant restorations, while awaiting review and re-torque of bridge screws at a later date, we irrigate the access channels with Clinisept+ prior to final filling with PTFE and glass ionomer cement or composite.
All the author’s patients now receive a pre-treatment 30-second Clinisept+ Mouthwash rinse prior to any invasive treatment. The idea being to reduce intraoral bacterial load. This should also help reduce the risk of contamination from airborne aerosol of micro droplets from patient’s mouths.
Post surgery
Implant patients receive detailed oral hygiene and maintenance care instructions. This includes using interspace brushes into the gingival sulcus around implants along with use of interdental brushes. Patients dip brushes in Clinisept+ to help effectively disinfect the gingival sulcus. Previously patients used chlorhexidine for this, but due to staining, only once or twice per week. Clinisept+ causes no staining, no mucosal irritation and is a much more effective antimicrobial. As such, daily use is possible. Moving forward it will be interesting to see how the use of Clinisept+ Mouthwash effects the long-term incidence of peri-implantitis. And also how effective its use is in the treatment of existing peri-implantitis.
Clinical Health Technologies also produces a hypochlorous solution for extra oral use, which contains a higher concentration of hypochlorous. The author uses the product for a number of ‘off label’ uses. Uses include hand washing and for disinfection of laboratory work and implant components such as abutments and crowns, bridges etc. With the product having such a high efficacy against bacteria, fungi, viruses and spores and doing so in an extremely short contact time, it should make an ideal hard surface disinfectant and is non corrosive. Patients use a spray version of the product. This disinfects their removable dentures as part of their denture hygiene regimen.

A real ‘game changer’
The specialist endodontist at the author’s practice advocates the use of Clinisept+ irrigation during root canal preparation rather than use of ‘bleach’ in cases where there is a risk of sodium hypochlorite entering the inferior dental canal. In such cases, were Clinisept+ to enter the inferior dental canal, it would not cause irritation or damage to tissues surrounding the apex of a tooth, or to the nerve tissue and blood vessels within the ID canal.
From the author’s point of view, and his patients’, Clinisept+ is a real ‘game changer’ and has completely replaced the use of chlorhexidine in so many areas of his daily practice of dentistry.
Disclaimer/statement of interest.
The author has received reimbursement for his time providing clinical feedback and preparing this article from Clinical Healthcare Technologies Ltd.
References
Pemberton MN and Gibson J (2012) Chlorhexidine and hypersensitivity reactions in dentistry. Br Dent J 213(11): 547-50
Smith JL, Drennan AM, Rettie T and Campbell W (1915) Experimental Observations ON THE ANTISEPTIC ACTION OF HYPOCHLOROUS ACID AND ITS APPLICATION TO WOUND TREATMENT. Br Med J 2(2847): 129-36
Let’s block ads! (Why?)






