 Simran Chaggar discusses the effectiveness of treating advanced periodontal disease with full arch dental implant rehabilitation.
Simran Chaggar discusses the effectiveness of treating advanced periodontal disease with full arch dental implant rehabilitation.
The prognosis for patients with aggressive periodontitis depends on a few factors:
- Whether the disease is generalised or localised
- The degree of destruction present at the time of diagnosis
- The ability to control future progression.
Early detection is critically important in the treatment of aggressive periodontitis. Preventing further destruction is more predictable than attempting to regenerate lost tissues.
The consequences of periodontal disease are one of the most common reasons patients seek full jaw rehabilitation with implants. These patients are often suffering physically, due to mobility, sensitivity and pain. They also suffer psychologically and emotionally because of how their smile looks.
They are constantly reminded of the extent of their dental disease. Every time they eat, clean their teeth, and involve themselves in any social activities. This has a drastic effect on their quality of life.
Evidence appears to support the use of dental implants in patients who have had aggressive periodontal disease. It is also important to recognise the risk of occlusal overload of dental implants when placed in periodontally compromised dentition.
Things to consider
The immobility of implants in a dentition that does not have a stable vertical occlusal stop may lead to implant overload. This is always considered when opting for full arch rehabilitation versus replacing the worst affected teeth only.
Full arch dental implant rehabilitation and fixed prosthetics can address some periodontal patients’ chief complaints. A stable fixed prosthesis gives them a level of function more like healthy dentition than their periodontally compromised teeth while also improving the appearance of the teeth.
Being a clinic that only does full arch dental implant rehabilitation, our objective is to ascertain whether the patient is suitable for such treatment or not.
Clinically, a patient’s dental condition must justify such invasive treatment, such as an edentulous patient or one that is obviously terminally dentate.
However, not all patients who have a clinical need for full arch treatment are necessarily suitable for it. The threshold is far more complex when considering the patient’s age, disease trajectory, motivation, quality of life, and most important, psychological preparedness to transition to prosthetic teeth.
Patient condition

After feeling unhappy for years, as a result of mobile teeth that caused pain and damaged the patient’s self-confidence due to their appearance, EH – a 37-year-old female – decided that enough was enough and that it was time to address her situation.
Fears over the only option being a denture or no teeth had resulted in the patient not seeking anything other than emergency treatment for the past five years. EH explained that she was due to get married. She wanted to enjoy the occasion. She wanted to smile for photographs and eat cake without worrying about her teeth.
EH referred herself. She researched potential treatments online, and booked in for a full clinical assessment at our Liverpool clinic. From a medical perspective, EH was fit and well, having given up smoking two years prior.
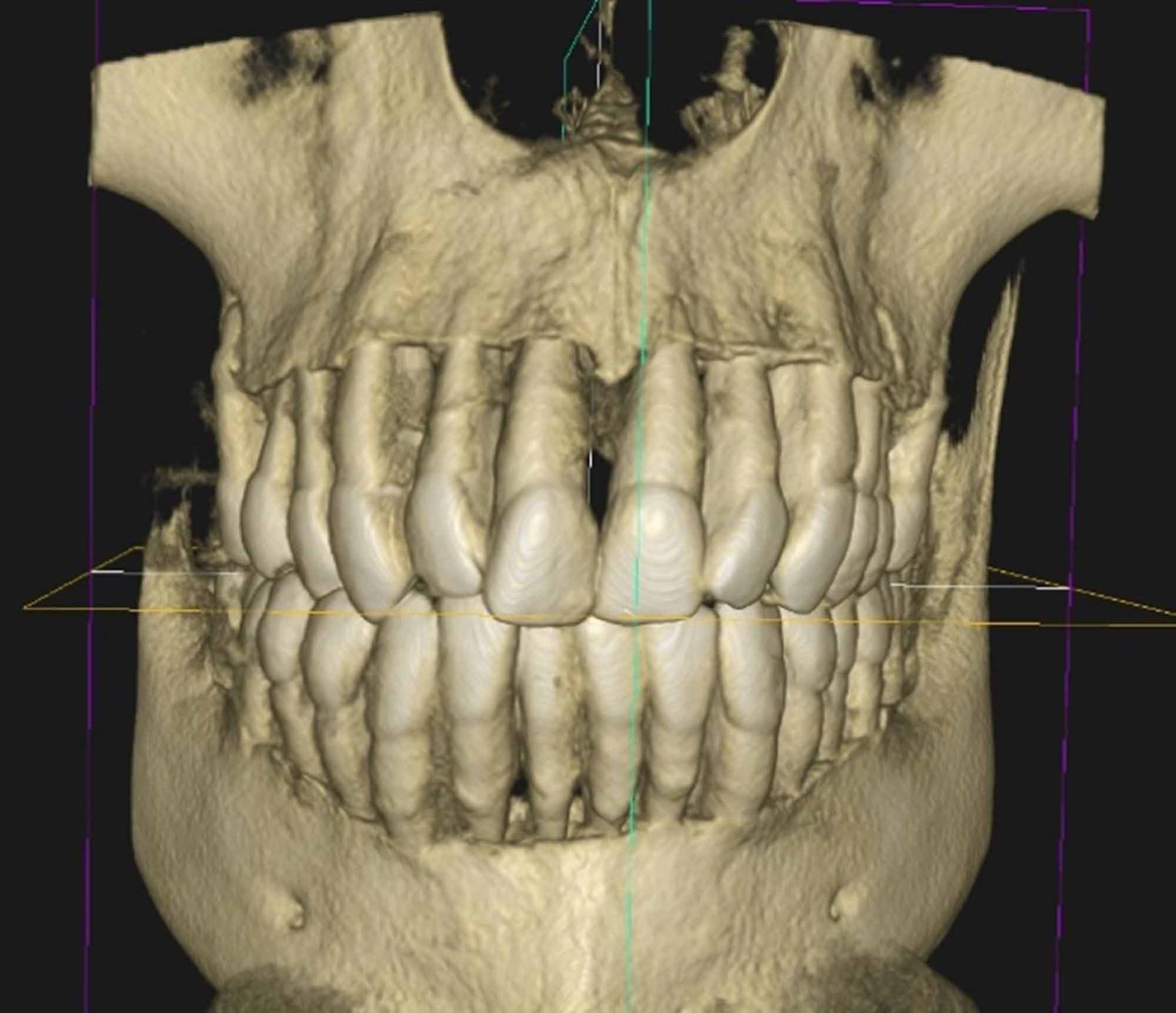
Following a full intraoral examination of the patient’s mouth and a cone beam computed tomography (CBCT) scan, the patient was diagnosed with aggressive periodontal disease, stage 4 grade C, with almost all teeth being grade 2-3 mobile. Aside from the periodontal disease, the patient’s dentition was unrestored.
CBCT
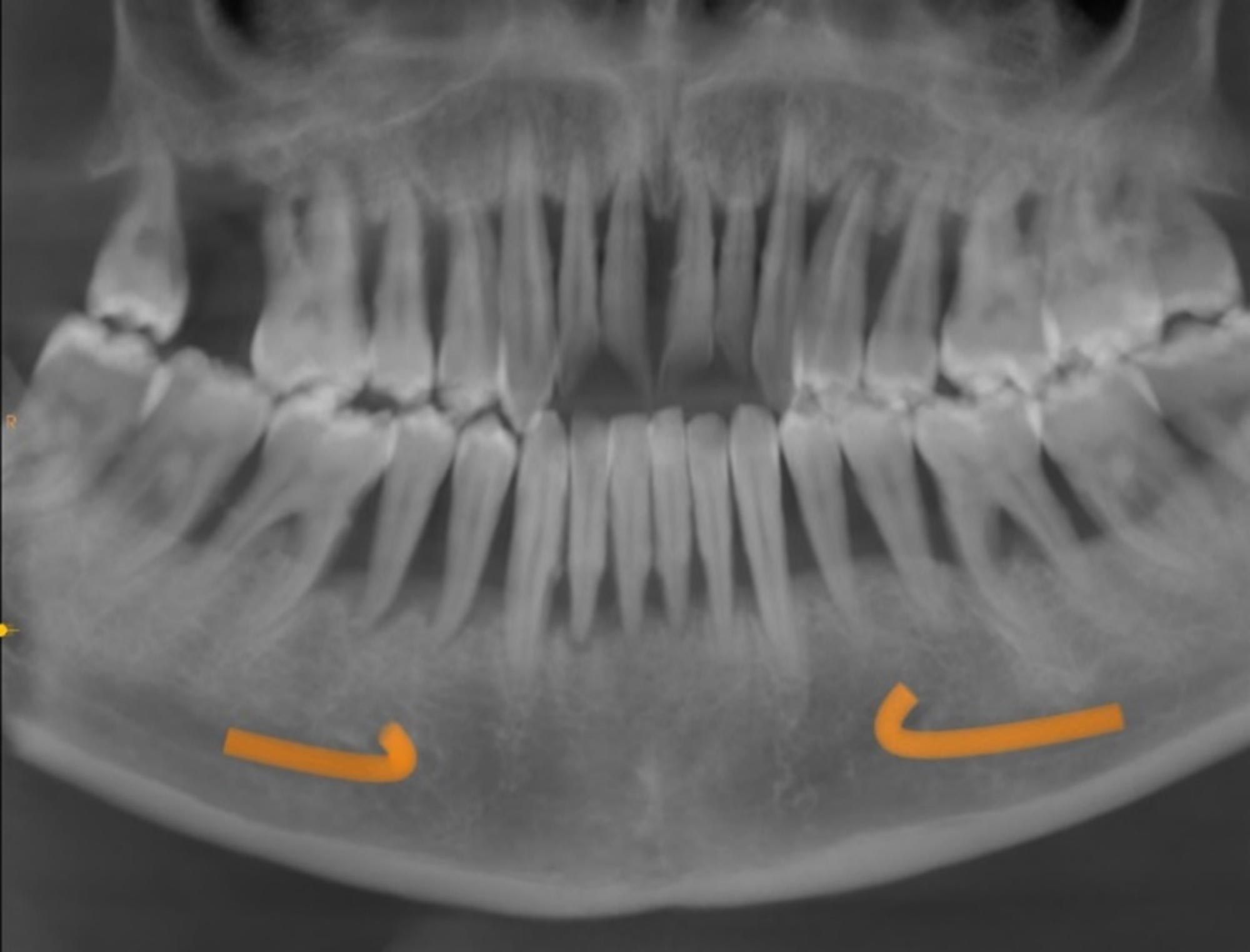
Her dentition was hopeless and the likelihood of stabilising and prolonging the life of her teeth was low. EH’s initial CBCT showed:
- Severe generalised horizontal bone loss
- Sufficient residual bone volume and quality for predictable immediate implant placement and immediate prosthodontic loading.
Following a multidisciplinary team meeting involving all clinicians and technicians, EH was presented with the options of:
- Returning to her periodontist for continued care and a transition into dentures and later, implants if appropriate
- Returning to her dentist to extract all her remaining teeth and provide full upper and lower dentures
- Finding a general implant dentist to extract all her remaining teeth and place implant-supported overdentures
- Graftless immediate-loaded fixed treatment, with a fixed transitional prosthesis fitted on the day of surgery and a definitive prosthesis fitted around six weeks later.
In presenting an option for fixed immediately-loaded teeth to EH, the point was laboured that her history of advanced periodontitis at a very young age would require her to accept the conditions necessary for a chance of long-term success with this type of treatment.
Prosthetic conditions
- Convex smooth intaglio surface without any flanges
- Fit surface elevated from the tissue creating a 1mm space that allows inspection of the transmucosal interfaces as well as facilitated access for oral hygiene aids such as interspace brushes and oral irrigators
- Acrylic gingiva that can easily be relined or trimmed to adapt to changes in the soft tissue architecture beneath the prosthesis
- A polished metal bar connection to the pterygoid implant with no teeth distal to the first molar, for easier cleaning.
Surgical conditions
- Sufficient time being spent degranulating and removing the infected soft tissues to ensure the implants are placed into a clean environment
- Contouring the irregular alveolus for optimal prosthetic design and hygiene
- Mucoplasty to thin down hypertrophic gingival tissues to eliminate pocket depths around implants and maintain equigingival or 0.5mm subgingival positioning of the prosthetic platform
- At least 10mm spacing between dental implants for easy cleaning between interfaces and preservation of bone that may be required in the future if revision surgery becomes necessary
- Fewer dental implants (four to six implants per arch) mean less transmucosal connections and less opportunity for bacteria to breach the prosthetic-biological interface, while offering sufficient biomechanical support for full-arch prosthetics.
After consideration, the patient did not wish to be edentulous for any period. She also did not wish to have a removable prosthesis.
The patient’s age and history of inflammatory disease within the gums was discussed at length. The patient was made aware that she will likely be having revisions over the years to keep supporting a fixed prosthesis.
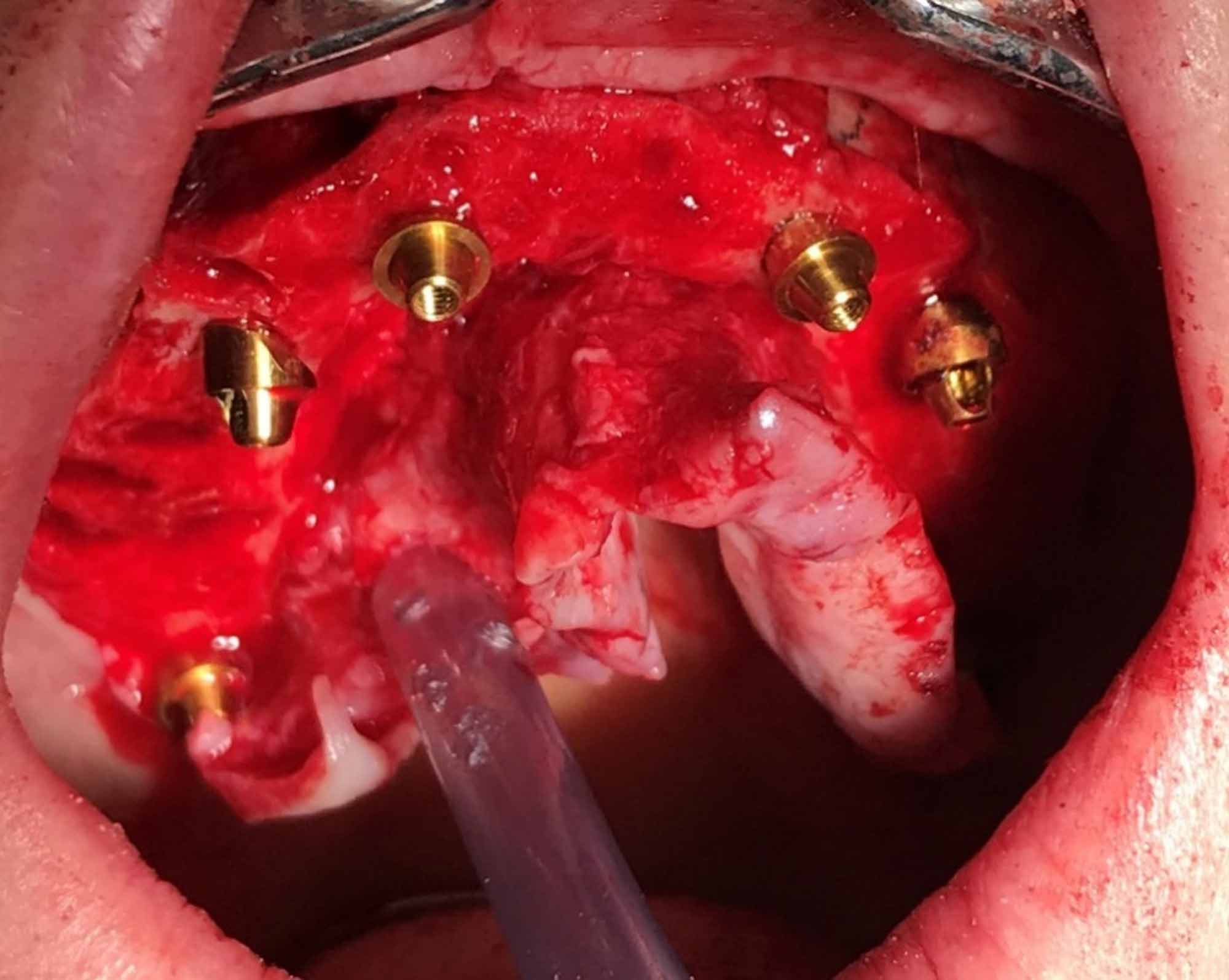
Surgery
The patient was under conscious sedation with IV midazolam. Due to the patient’s teeth being so loose, I opted to start by extracting the posterior teeth as they would interfere with pterygoid placement and impression taking. There was the added benefit that with a more limited mouth opening it would be difficult to treat the upper arch without the lower teeth interfering.
I then proceeded to start the upper arch, working on the right-hand side, extracting (UR8-1) and keeping the teeth on the left-hand side alongside a few lower teeth on the left and side for stops.
I was expecting more bleeding from the granulation tissue; however I was fortunate the patient did not bleed as much as expected.
I raised a full thickness flap to expose the distal end of the alveolar crest. I started to clean all the granulation tissue and prepare the crestal bone for implant placement.
We used Tapered External-Hex MSC surface implants (Southern Implants, SA) for EH, which feature a hybrid surface configuration of roughened implant surface to enhance bone growth onto the implant while the coronal 3mm, and collar of the implant, are left as machined (ie, smooth), helping to prevent plaque and biofilm forming that lessens the risk of peri-implantitis.
The upper right pterygoid, UR4 and UR2 were all placed first with an insertion torque of 50Ncm, all with apical cortical engagement.
Alveoplasty
I then edentulated the left-hand side, degranulated, prepared the bone for placement and proceeded to place the upper left pterygoid, UL4 and UL2 at 50Ncm. The patient was compliant and relaxed during the procedure.
Mucoplasty was performed to thin down the soft tissue. The palatal flap was re-positioned buccally for keratinized tissue around the implants, to act as a first line of defence against a harsh oral environment.
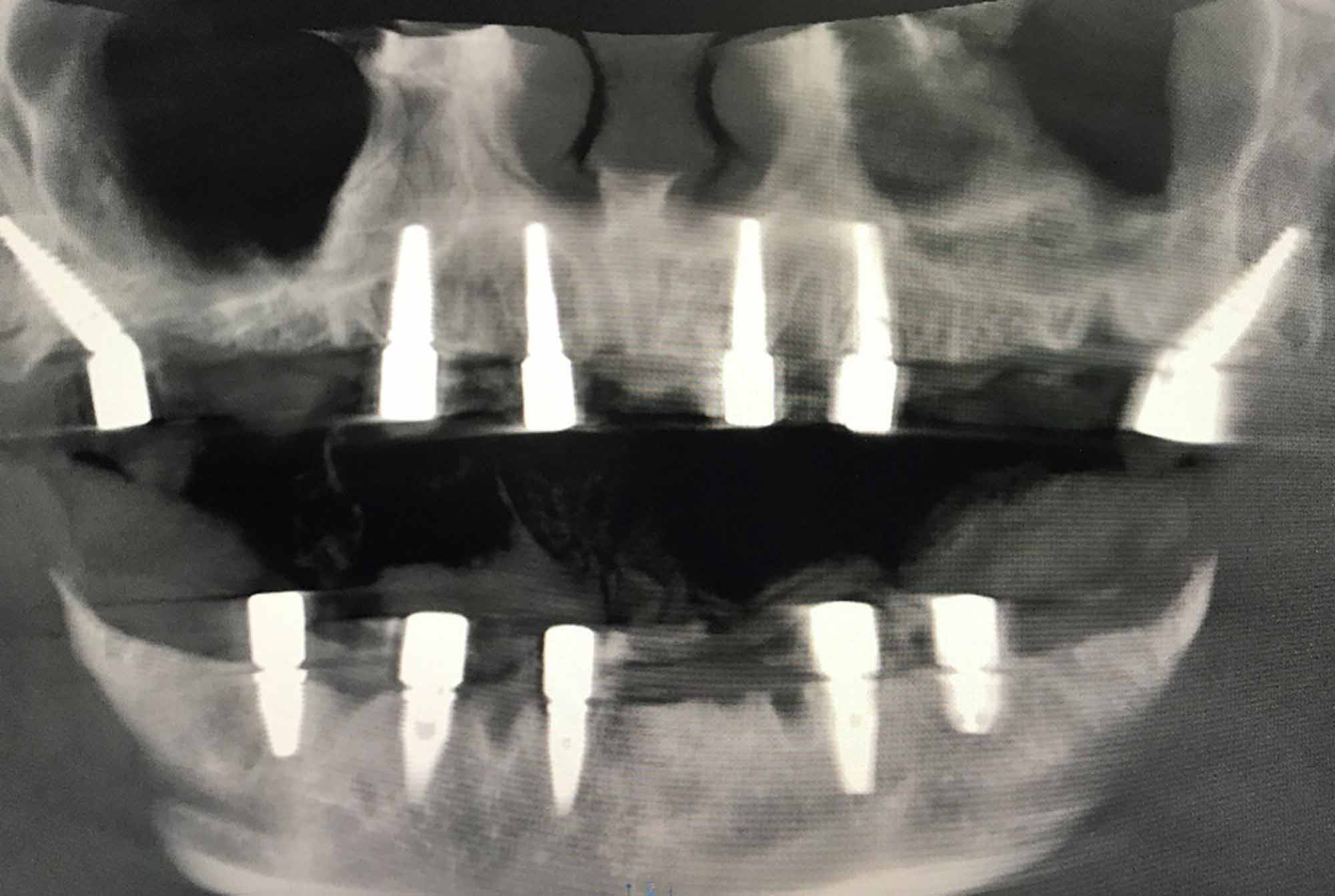
A plaster multi-unit abutment level open tray impression was taken. The patient was then given a short break along with 400mg of ibuprofen. I closed with 4-0 Vycryl Rapide Sutures. The lower jaw followed with extraction of the remaining lower teeth. I raised a full thickness flap and exposed the mental nerves on both sides, marking their locations.
An alveoplasty was performed to create adequate restorative space. Also, to ensure a flat cleansable platform for the prosthesis to sit on. A considerable amount of time was spent on degranulation, followed by placing the implants from back to front. Closure and plaster impressions were then taken.
Immediate fit
As with all of our patients, EH was provided with her own suite for the day. Here, she was monitored post-sedation and rested while waiting for the polymethyl methacrylate (PMMA) prosthesis to be milled to interface.
The temporary prosthesis was fitted with an adequate aesthetic and functional outcome. The patient was very happy with the result.
Postoperative instruction was given and the patient was discharged to be reviewed in three weeks; at which point the soft tissue healing, function and aesthetics would be assessed.
Definitive fit
The patient was fitted with final prosthetics at seven weeks, constructed of PMMA with a titanium substructure; for increased strength.
At this stage, she is still on softer foods. However, the treatment has addressed the two main factors that were detrimental to her quality of life.
EH now feels confident to smile and laugh in public again. She can eat and clean her prosthetics without experiencing pain. EH is now incredibly excited for her wedding later in 2021.

Hygiene and postoperative
EH received thorough oral hygiene instructions and the necessary aids to maintain her peri-implant health. She was also given a demonstration and a manual on how they are used.
She was given a maintenance schedule, which involves quarterly visits to the clinic for examination of hard tissue, soft tissue, implants and prosthetic that will allow for early identification of problems and intervention as required.
Conclusion
To justify carrying out a procedure like a full arch dental implant rehabilitation, you must meet the clinical and psychological thresholds.
The standard procedure at Evodental clinics is to issue the final treatment plan following a multidisciplinary team meeting involving the entire clinical and technical teams.
This ensures all angles of treatment need, prosthetic design, surgical complexity and treatment alternatives – including non-implant options, or solutions involving grafting, delayed loading or removable prosthetics – are considered.
Most cases, like EH, are clear cut with a definite disease trajectory towards total dental failure. Others are ‘borderline’ where additional considerations come into play:
- What degree of dentistry would a patient have to endure to ‘save’ or prolong their teeth?
- What would the cost be?
- How easy would it be to maintain?
- What is the likelihood of success?
This will certainly include consideration of the patient’s age, medical history and financial capability. Ultimately, you must find a balance. One that offers a patient treatment solutions that give them stable oral health, function and quality of life. After that, you should respect their decision.
To learn more about Evodental, visit the ‘for dentists’ section at www.evodental.com.
This article first appeared in Implant Dentistry Today magazine. You can read the latest issue here.
Let’s block ads! (Why?)






